Antibody therapies for COVID-19
Produced by Jack Lee, Science Communications program UCSC.
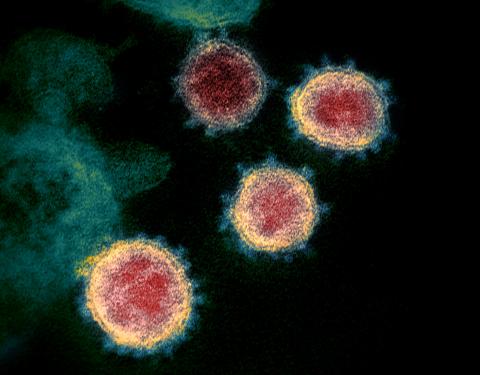
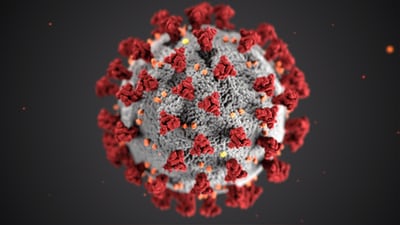
Scientists are racing to develop treatments for COVID-19. Some of these remedies might not look like tablets or capsules: They could be antibodies that doctors inject directly into our veins. These antibodies would be like the ones floating around in our immune system. But these ones would target proteins that make up the coronavirus that causes COVID-19 and stop the virus in its tracks. I’m Jack Lee with a look at the potential — and possible shortcomings — of antibody medicine.
When we’re infected by viruses — like a cold or the flu — our immune systems respond by producing antibodies. These Y-shaped proteins attach to bacteria and viruses that have invaded our bodies and flags them for destruction by immune cells.
Antibody therapies are trying to do the same thing. Lena Meyer is a graduate student in the DuBois Lab at UC Santa Cruz. Her lab studies how antibodies can block viruses from infecting cells.
Meyer: Monoclonal antibody therapy has been used for a couple of different diseases, mostly in cancer or autoimmune diseases. And that’s because in those diseases you can characterize a specific molecule that you want antibodies to target.
Monoclonal antibodies are produced in labs, rather than human bodies. Unlike the mix of antibodies in our immune systems, these ones are identical and attach to the same protein.
For RSV, a virus that causes airway infections in infants, researchers have developed a monoclonal antibody that targets a protein on the outside of virus particles. By sticking to these surfaces, the antibodies prevent viruses from getting into human cells.
Antibody-based treatments may have some advantages over treatments using chemical drugs.
Meyer: Antibodies actually have lower off target effects than small molecule drugs. Because, by definition, antibodies are really specific for binding to only one thing.
But there are also tradeoffs.
Meyer: Some disadvantages of antibodies are that they are really large. So, they’re both hard to produce in the lab and also hard to administer to patients.
It’s also a challenge to make sure that a monoclonal antibody attaches to the right place on a coronavirus particle to block it from entering human cells.
Another way that researchers can quickly get lots of antibodies that target coronavirus proteins is by going to a different source: patients who recovered from COVID-19 and have already mounted an immune response.
Meyer: The hope is that because Coronavirus hasn’t been studied long enough for there to have been time to develop a monoclonal antibody therapy, we could instead use convalescent plasma, which contains a pool of different antibodies. A good proportion of them hopefully target the coronavirus.
Plasma is the liquid part of our blood — as opposed to red blood cells, white blood cells and platelets. It has a mix of antibodies targeting a whole assortment of different proteins. The hope is that in that mix, there will be some that prevent the coronavirus from getting in our cells.
Convalescent plasma therapy involves sucking out one person’s plasma — with antibodies that attach to coronavirus proteins — and injecting it into others.
Pandey: One plasma donation from a single donor will get split into, you know, smaller components, plasma components that can be used to treat three to four patients.
Dr. Suchi Pandey is the chief medical officer for Stanford Blood Center, which has started collecting plasma from patients who have recovered from COVID-19.
This might all sound like something out of a vampire movie, but it’s actually sound science. The approach has been used in the past, for treating diseases like the flu. It’s also safe.
Pandey: We transfuse plasma all the time in the hospital setting and because of just all of the advances in blood safety, blood and plasma transfusions are considered to be very safe.
It’s important to keep in mind that convalescent plasma is only a short-term measure because the provided antibodies don’t last forever. The donated plasma is just a stopgap until the recipient’s immune system ramps up antibody production.
Hospitals have already started providing sick COVID-19 patients with convalescent plasma through compassionate use programs, also known as expanded access.
Pandey: Stanford Hospital is able to provide products to patients in the expanded access protocol and has provided patients already within that protocol. And they are gearing up to start a clinical trial in the next few weeks.
Convalescent plasma seems to be helping seriously ill patients. But to know for sure that convalescent plasma helps, we need to wait for the results of formal, randomized clinical trials. It’ll be a few months until we find out the results, but recovered patients are already having an impact now.
Pandey: I think it has been really inspiring to be able to meet the donors and understand the illness that they went through. And now that they’re better, really being motivated and wanting to help other patients that are currently battling COVID-19.
People who want to donate plasma can visit Stanford Blood Center’s website and fill out a form to participate in their convalescent plasma program. I’m Jack Lee with this science report